Telemedicine and telehealth — do you recall the first time you heard those terms? For most ordinary Americans, our guess is that you’ll say around March or April 2020. That’s when some mysterious, deadly illness started hitting U.S. shores. Suddenly, businesses were closed, toilet paper shelves were bare, and an app called Zoom rushed to the top of Apple and Android store downloads. It all seemed to happen at the speed of light.
When Telemedicine Went from Just Talk to All Talk
The truth is, telemedicine (or telehealth) is something that insurance companies, doctors, and consultants that work on both sides have been discussing for years. There are pros on both sides and only minor cons. It’s more affordable for doctors and patients to meet online for quick checkups. Also, if doctors could relegate a percentage of patients to telemedicine appointments, they can see more patients per hour and invest more time in providing good health care.
There is a different slew of benefits for patients. Dialing-in to doctor appointments is safer for a lot of people, like the elderly and patients with mobility or transportation issues. Plus, they can miss fewer appointments when they’re feeling under the weather or can’t secure a ride. And for patients who are too sick to leave the house, a telehealth appointment is much safer for themselves and the community. Parents love telemedicine because the time saved on appointments is one less missed day of work, missed school, or activities for kids. Basically, everyone benefits from telehealth.
The most cited downsides are from individuals who don’t have a smartphone or computer or are intimidated by the technology.
Here is one topic almost everyone agreed on: if implemented, telemedicine would save money and save lives. It would be a win-win for everyone.
How Telehealth Saves Lives & Money
The pandemic hit in early 2020. It’s not that Covid suddenly threw the country into a new way of thinking about or disseminating health care, it’s just that while the infrastructure was in place, people had to learn a few new skills. At that time, it wasn’t unusual for a percentage of the population to be brand new to teleconferencing and the software it requires. That’s the part that happened at warp speed. And nothing at that caliber ever gets done that fast. But thanks to a contagious pandemic, there was no choice. The only problem left was that telemedicine was not yet part of consumers’ vocabulary.
While some doctors and practices had used technology, like Skype and FaceTime, for short chats with patients, most had not. There were also crucial laws that medical professionals were concerned about. For example, general practitioners and specialists worried about whether it was safe to talk about patients’ health status and treatment plans over the internet.
And mental health providers? They were more concerned than almost any other health provider. Not only is there still a major stigma surrounding mental health care and treatment, but even in the 2020s, therapists had no idea whether it was safe to have sessions online. Topics like depression, eating disorders, domestic abuse, suicidal ideation, and prescribing psychotropic medications would inevitably be discussed during online therapy.
Two Years is a Lifetime in Telehealth Years
Now it’s more than two years since those early telemedicine days and it’s like the world evolved by decades. Today, providing medical treatment online is just another way for doctors and patients to interact. So at Decoding Health Insurance and the Alternatives, we thought we’d look at some of the progress the modality made since those early days of 2020 when the world suddenly felt like it was coming to an abrupt and scary end.
Facts about Telemedicine
Here are some interesting factoids we uncovered:
- The U.S. Department of Health and Human Services (HHS) found that massive increases in the use of telehealth helped maintain health care access during the pandemic and after.
- Even in December 2021, just over six months after living with Covid, HHS reported a 63-fold increase in telemedicine use.
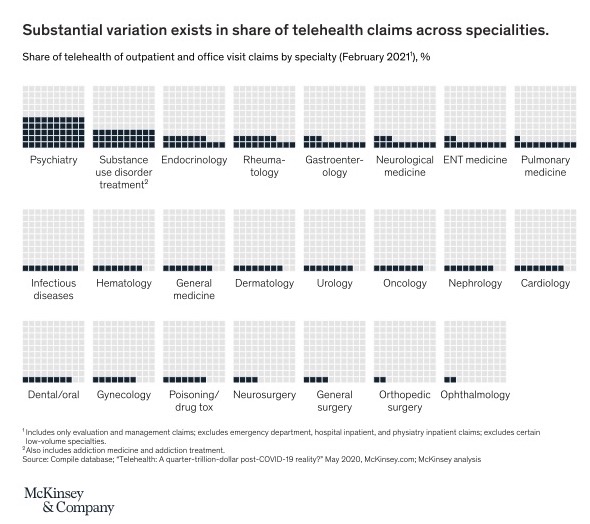
- Early in the pandemic, specialists were seeing more patients than general practitioners. To get the virus under control, some governors canceled in-office elective procedures and surgeries. So face-to-face online visits with specialists were the only way people with certain health conditions could receive treatment.
You Like Telehealth!
Do you know who really knows if telemedicine was a good idea? Real people! We found an AARP article — granted it’s from 2020, before social distancing, canceled elective medical procedures, and homeschooling in lieu of on-site learning. But for certain communities, like rural areas and the elderly, telemedicine was already making a lot of progress. So here’s what some people had to say about dialing-in — rather than driving — to their doctor appointment.
Real Telehealth Stories
- A 69-year-old from South Carolina who spent a lifetime sitting in medical waiting rooms for doctor appointments begrudgingly agreed to a virtual urologist visit. To her surprise, she managed to download an app on her cell phone and her doctor called prescriptions into her pharmacy. In less than 15 minutes, the appointment was over. And there was no waiting room, no commute, no doctor behind on his schedule. “Normally, I would have to get in my car and drive a half-hour and wait in the office and then get back in the car and drive home. That takes half a day.”
- In Montana, a 62-year-old recently had hip surgery. This time, it was her doctor who was new to teleconferencing. The Billings-based development coach had been talking with clients online for years by this point. During her first telehealth appointment, the doctor asked about post-surgery symptoms, reviewed her medications, and talked about ways she could manage her blood pressure. The patient said, “It felt like we were eye-to-eye.” Now that patient is hooked on doctor visits from the comfort of her own home. “As you get older, you’re more likely to have mobility issues,” she said.
- A Pennsylvania man in his 60s was extremely worried about getting the new virus going around. His immune system was weakened from prostate cancer. On his first telehealth call, his doctor and nurse were present. The patient asked questions about his disease and how to avoid catching that other, scarier, illness. He told a reporter at AARP, “I’m not a real techie with computers, but I did OK.” The best part? Just to be safe, he sat at his computer five minutes early. It was the shortest amount of time he ever had to wait to see the doctor.
Telehealth Improves Medical Care
People who live in rural areas, especially those in health professional shortage areas (HPSA), are sure to benefit from this form of health care the most. In a recent report by AARP, 10% of adults who live outside of the suburbs have lost a local hospital or medical clinic and a fifth don’t have specialists in their communities. We’re talking oncologists, cardiologists, neurologists, and many more. So in November 2021, they published an article, 3 Ways Telehealth Can Improve Medical Care in Rural America. Here are the highlights:
Ways Telehealth Improves Care for Rural Americans
- It’s easier for those who live miles and miles from big cities and suburbs to see doctors and specialists. Roughly a quarter are forced to travel more than 31 minutes to get to a specialist’s office.
- Patients with chronic illnesses are more likely to get care. Telehealth reduced hospital admissions and emergency department visits. Heart patients learned to take their own blood pressure, and those with diabetes learned to do their own blood-sugar readings. After sending results to their medical team via telehealth, doctors can adjust medications and treatments from and to almost anywhere.
- Most doctors who live in rural areas are general practitioners. When a patient with a complex medical problem comes into their office, they can’t always provide treatment. However, that doctor can find specialists at an advanced research institute (usually located in large urban cities) and get help treating a variety of diseases. In the past, those same doctors would have to refer patients to doctors that might be a hundred miles away or more.
Pay Per Visit
The truth is, while Zoom doctor appointments may have made it easier to treat and increased mortality for more patients, it didn’t make it any easier to get health insurance. Most people still either need a job that helps pay for a comprehensive health insurance plan or earn enough money to get a private plan or one through the health care marketplace. With telehealth, people have so many more options.
According to Lauren Jahnke, author of Decoding Health Insurance and the Alternatives, “People without insurance can subscribe to a telemedicine health plan or pay per visit, while people with group or individual insurance may pay for services or be provided with free access to telemedicine through their health plan.” Jahnke, an author with more than two decades of health policy experience, writes about telemedicine in chapter 10 of her book. She talks about the advantages of telehealth, state regulations, and even lists a few of the many telemedicine companies that have been cropping up in the past few years. (As we said early in this article, telemedicine has actually been around quite a while even though it’s still a new concept to most ordinary Americans).
Where to Get Online Health Care
Here are a few telehealth companies that offer per-visit pricing:
- BetterHelp– This is an online mental health provider. Patients pay about $60 to $90 per week, which is well below the cost of seeing a psychologist or certified social worker (CSW) in person. Patients can get help for depression, anxiety, relationship problems, trauma, and many other mental health problems and disorders. They can even get prescriptions.
- Doctor on Demand – This online health provider treats urgent care, preventive care, and chronic care issues, like allergies, cold & flu, hypertension, IBS, and provides medication management. At Doctor on Demand, patients can choose their own provider, which is a huge benefit. Like with any medical visit, costs vary depending on insurance status. But a 15-minute consultation with a board-certified clinician (about the same amount of time you’d get with a doctor at an office) is $75.
- Teladoc – This integrated virtual care system delivers “whole-person health — from wellness and prevention to acute care to complex health care needs.” For someone who doesn’t have insurance, a general medical visit with a provider from Teladoc can cost about $75 per visit, or $0 for a patient with insurance.
Check Out Decoding Health Insurance
To better understand the U.S. health care system, check out Decoding Health Insurance and the Alternatives: Options, Issues, and Tips for Saving Money. And for more information specifically about telehealth, go to chapter 10 of the book. You’ll find easy-to-read information, plus tips for where to see a health care professional from the comfort of your own home.
See our Partners Page for a look at additional help you can find in the health care industry.
And learn much more about the health insurance landscape at decodinghealthinsurance.com, by reading our blog, and signing up for our newsletter.
